BY: SAI MANOGNA (MSIWM014)
The significant majority of cells involved in the immunity of mammals are derived from the bone-marrow precursors (Left half of the figure) and circulate in the blood, entering if possible and leaving the tissues. In the adult bone marrow at a frequency of 1 in 100,000 cells, an intermittent stem cell survives and maintains the potential to differentiate into all blood cell forms.
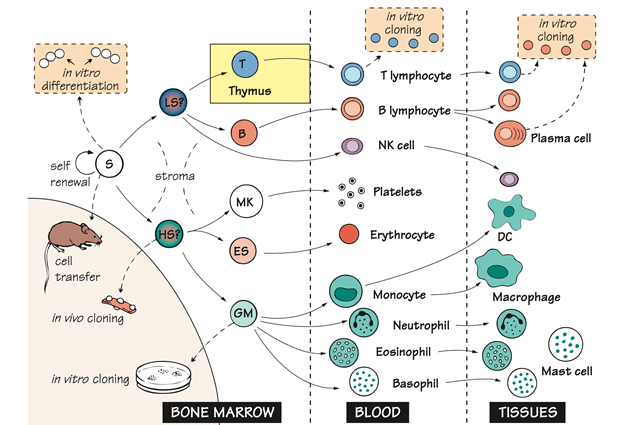
Haemopoiesis has been studied either by injecting a group of cells into the recipient mice of genetically marked marrow cells and examining the progeny they give rise to (Invivo cloning) or by cultivating the bone marrow precursors in the presence of sufficient growth factors (Invitro cloning).
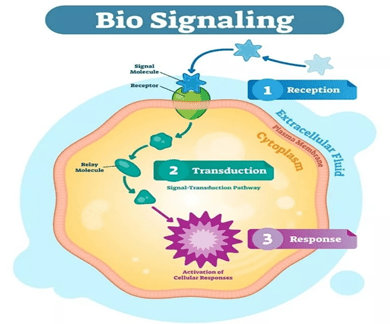
The proliferation and differentiation of all these cells is regulated by the soluble membrane bound growth factors that usually generate the stroma of bone marrow and each other. Such signals turn-on the particular growth factors inside the cell, DNA binding molecules that serve as master switches, establish the subsequent genetic program, resulting in the production of various types of cells.
Bone Marrow :
Unlike any other tissues or organs, the hematopoietic system continues to regenerate itself. In adults hematopoietic cell production occurs primarily in the bone marrow. In the fetal hematopoiesis occurs first in the yolk sac and then in the liver until the bone grows.
Stroma : In haemopoiesis, epithelial and endothelial cells that provide protection and secrete growth factors.
Lymphoid stem cell : These cells are assumed to be capable of differentiating into B lymphocytes and T lymphocytes. Recent research findings indicate that the distinction might actually be more complex between lymphoid and myeloid stem cells.
Haemopoietic stem cell: Spleen nodule precursors are presumably capable of differentiating into all but lymphoid pathways i.e, granulocyte, erythroid, monocyte, megakaryocyte, also referred to as CFU-GEMM. CFU-GEMM refers to the colony forming unit that generated myeloid cells. GEMM refers to Granulocyte, Erythroid, Monocyte, Megakaryocyte.

Erythroid Stem cell : These erythroid stem cells generate erythrocytes. In response to hypoxia, erythropoietin, a glycoprotein hormone produced in the kidney, hastens the differentiation of red cell precursors, and thus adapts red cell development to the demand for its oxygen carrying capacity which is an example of NEGATIVE FEEDBACK.
Granulocyte–Monocyte : This is the common precursor. The growth or colony stimulating factors influence the relative proportion of these two types of cells.
Cloning : By isolating the single cells and allowing them to differentiate several times, and then studying what cell types can be found in the progeny. Thus the ability of individual stem cells to give rise to one or more types of hematopoietic cells has been explored. This approach is referred to as cloning. A clone is a group of daughter cells originating from the single parent cell. These evidence indicate that a single stem cell can give rise to all the fully differentiated cells of an adult hematopoietic system under specified conditions.
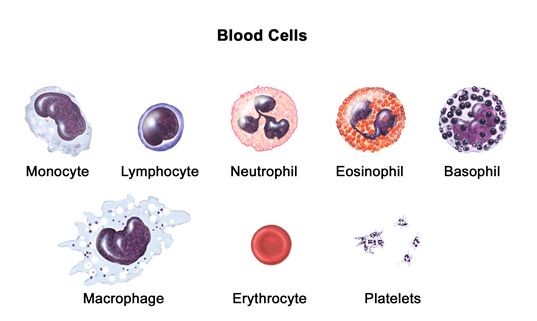
Neutrophils : These are the short-lived phagocytic cells whose granules contain voluminous bactericidal substances, is the most prevalent leukocyte in the human blood. The first cells to exit the blood and to enter the sites of infection or inflammation are neutrophils.
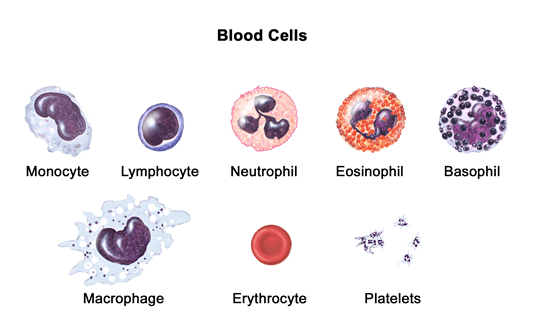
Eosinophils : Eosinophils are the leucocytes with large refractile granules, containing a number of proteins that are highly basic or cationic proteins possibly essential for the killing of large parasites, including worms.
Basophils : These are the leukocytes with large basophilic granules containing heparin and vasoactive compounds which are essential in inflammatory response. The three types of cells which are neutrophils, eosinophils and basophils are collectively known as GRANULOCYTES.
Megakaryocyte : These are the parent cells of the blood platelets.
Platelets : These are the small cells which are responsible for sealing the damaged blood vessels (Which is known as haemostasis) but these cells are also the source of several inflammatory mediators.
Monocyte : The mononuclear phagocytic system consists of monocytes. Monocytes circulate in the bloodstream for about 8 hours and then migrate into the tissues. When these migrate into the tissues, they differentiate into specific tissue known as macrophages. Additionally monocytes are drawn to inflammation sites, replenishing a reservoir for macrophages and possibly dendritic cells as well.

Macrophages : Macrophages are strewed throughout the body. In specific tissues some take up residence, becoming fixed macrophages, while others remain motile called as free or wandering macrophages. These free macrophages migrate across the tissues by amoeboid movement.
Macrophage like cells serve various functions in different tissues and these are named according to the site of location;
Kupffer cells in Liver
Osteoclasts in Bone
Alveolar macrophages in Lungs
Mesangial cells in Kidney
Intestinal macrophages in Gut
Microglial cells in Brain
Histiocytes in Connective tissue.
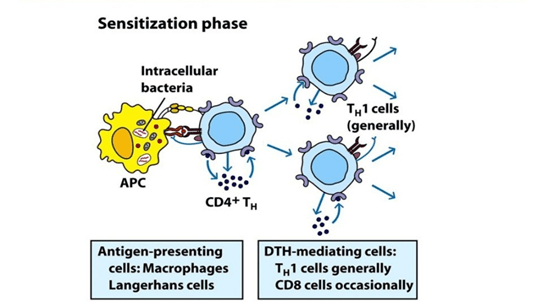
Dendritic Cells : Dendritic cells are present in all body tissues (eg; Skin cells of Langerhans) where they pickup the antigen and then migrate through the lymphatics or the blood to the T-cell areas of lymph nodes or spleen. Their main function is to activate T-cell immunity, but they might also be involved in the induction of tolerance as well. The plasmacytoid DC is the name derived from their morphological resemblance to the plasma cells. The second subset of these cells are the principal producers of type I interferons, which is an essential group of viral proteins. Experimentally, while these cells are derived from the myeloid cells, the developmental lineage of bone-marrow dendritic cells is still the subject of debate.
Natural Killer Cells (NK Cells) : NK cells have been shown to play a significant role in host defence against both tumor cells and cells infected with certain, but not all the viruses. The membrane molecules and receptors that differentiate T and B cell lines do not express these cells. These cells make up 5%-10% of lymphocytes in the human peripheral blood.
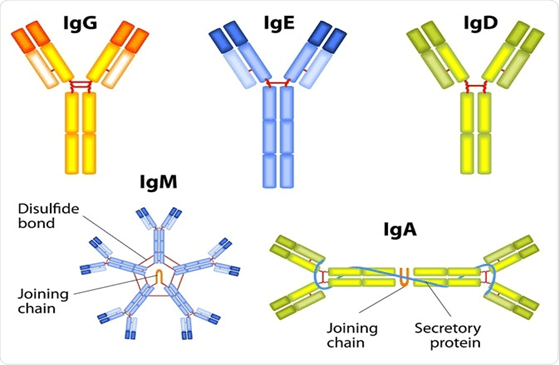
T and B Lymphocytes : These cells are main cellular components of adaptive immunity. T-lymphocytes are derived from the thymus, while B-lymphocytes are derived from the bone marrow of birds or bursa derived. The precursor for antibody forming cells is B-lymphocytes. The liver may play the part of bursa in the liver.
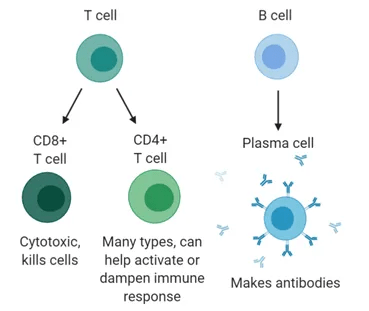
Plasma Cell : Plasma cells are rarely seen in blood. These cells are present if an antibody is formed in the spleen, lymph node etc; Plasma cells do not differentiate and cannot be retained invitro for extended periods. B lymphocytes that generate particular antibodies may however be fused with a tumor cell to generate an immortal hybrid clone or hybridoma that continues to secrete a predetermined range of antibodies. As unique instruments in many branches of biology, such monoclonal antibodies have proven to be of immense benefit and some are now being widely used for the treatment of autoimmune disorders or cancers.
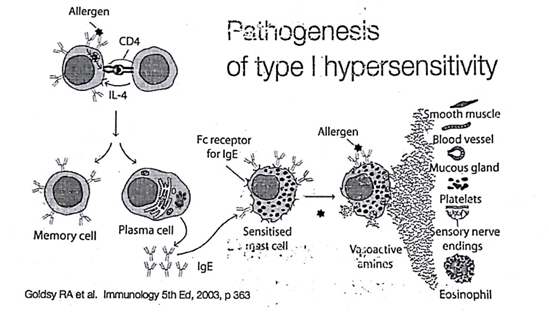
Mast cells : Mast cells are the large tissue cells that are derived from the circulating basophils. To start an inflammatory response, that causes several types of allergy, these mast cells are rapidly activated by tissue damage.
Growth factors : The molecules that regulate hematopoietic cell proliferation and differentiation are also often involved in the regulation of immune responses, such as interleukins or cytokines. In these some of them were first discovered by hematologists and are referred to as Colony stimulating Factors (CSF), but there is no particular meaning to the various names, and one ; IL-3 is sometimes referred to as multi-CSF. In clinical practice growth factors are used to improve specific blood cell subsets and erythropoietin was one of the first proteins developed by recombinant technology in the modern century.